Regain Control. Live Confidently.
Effective, modern treatment options for mixed urinary incontinence (stress + urgency).
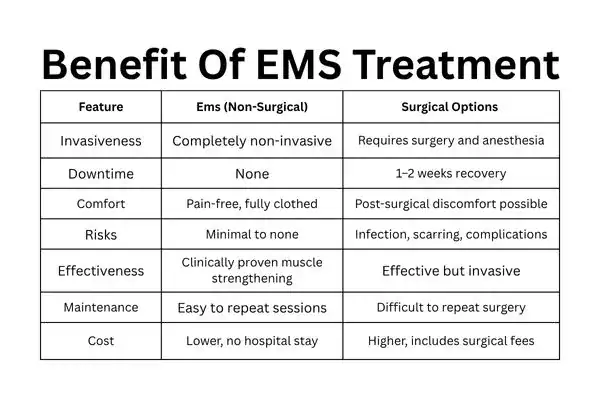
Whether you leak when you cough, laugh or have sudden, urgent trips to the bathroom, there are non-surgical and surgical options — including a cutting-edge, non-invasive electromagnetic therapy called EMS.

Mixed urinary incontinence (MUI) is leakage that has characteristics of both stress urinary incontinence (SUI) — leakage with physical exertion — and urgency urinary incontinence (UUI) — leakage associated with an acute, unprompted urge. Management typically begins with conservative measures (lifestyle changes and pelvic-floor muscle training) and progresses to devices or surgery when symptoms remain.
Conservative first: Bladder training and supervised pelvic-floor muscle training (PFMT) are first-line choices.
Device-based, non-invasive: high-intensity focused electromagnetic (HIFEM) therapies (e.g., EMS) build pelvic-floor strength without invasive ut probes or surgery. There is evidence of improvement in SUI, UUI and mixed symptoms among many patients.
Surgical: mid-urethral slings and other surgeries work for SUI and induce lasting symptom improvement, but they are invasive with the consequences of surgical risk and recuperation time. Data from clinical guidelines and RCTs with long-term follow-up suggest even greater reductions in long-term symptom levels among selected surgical patients.
The EMS chair treatment uses electromagnetic energy to trigger powerful pelvic floor muscle contractions, helping women of all ages strengthen their pelvic floor muscles and pelvic muscles, improve bladder control, and reduce urine leaks caused by stress incontinence, urge incontinence, or pelvic organ prolapse—supporting daily activities and overall confidence, while addressing individual needs, minimising dependence on incontinence products, and being guided safely through every step of the way with awareness of any possible risks; complementing traditional pelvic floor exercises and care for related medical conditions.
EMS uses pulsed electromagnetic fields (HIFEM) delivered through a chair to stimulate pelvic-floor neuromuscular tissue and cause involuntary, supramaximal pelvic-floor muscle contractions. Those contractions are intended to improve muscle strength and neuromuscular control — similar in effect to many Kegel exercises but performed non-invasively. Clinical trials and device evaluations report improvements in the frequency of leakage episodes and quality of life for many patients.
Typical Mixed Incontinence Treatment Course
Protocols vary by clinic and by study. Standard real-world courses are six sessions (about 2 per week over 3 weeks), or protocols used in some trials are 6–8 sessions. Your clinician will confirm a personalised plan based on symptom severity and response.
Safety & who should avoid EMS
EMS is cleared by the FDA (510(k)) for the treatment of urinary incontinence; it’s generally well-tolerated. Contraindications commonly include pregnancy, implanted electronic devices (e.g., pacemaker, ICD), certain metallic pelvic implants and active pelvic infection. Muscle soreness and tingling are common, mild, and temporary side effects.
As with any therapy, discuss medical history and devices with your clinician.
Overactive bladder is one of the most frequently observed types of urinary incontinence, causing a sudden urge to urinate, urine leakage and disruption to daily life — specifically in people with weak pelvic floor muscles, limited mobility or other health conditions that affect the urinary tract or bowel function.
Age-related problems with the pelvic floor, hormonal changes and the physical consequences of overactive bladder syndrome, overflow incontinence or accidental leakage of urine when the bladder is full during bowel movement can all be treated through pelvic floor muscle training, specialist nurses or electromagnetic technology—all effective solutions that have been proven to improve sexual health and overall quality of life, countering social isolation while safely addressing various concerns about types of urinary incontinence accompanied by advice on dealing with potential risks, litres/frequency/what now poops-volume/intake pressure requirements or any further questions regarding one’s specific type urinary incontinence prior.
Q: Is EMS FDA-cleared?
A: Yes — EMS has 510(k) FDA clearance for treating urinary incontinence and is widely used in clinics; manufacturers and regulatory documents confirm clearance. Like any other medical device, have your clinic provide its regulatory and clinical documentation.
Q: How many sessions will I need, and how long do they last?
A: Normal courses are 8-10 sessions (around 28–30 minutes each), typically run 1–2 times per week. You should customise the plan with your clinician.
Q: Is it painful?
A: Most patients report sensations of pelvic-floor muscle contractions (some describe it like an intense Kegel), with minimal discomfort. Occasionally, there’s short-lived muscle soreness afterwards.
Q: How soon will I notice improvement?
A: Some people notice improvements after the first few sessions; for others, it takes the whole course. Degree and timing of benefit vary by individual and symptom type. Trials report symptom and quality-of-life improvements in many participants.
Q: Are there people who should NOT have EMS?
A: Yes — contra-indications commonly include pregnancy, implanted electrical devices (e.g., pacemaker/ICD), metallic pelvic implants, and active pelvic infections. Always review full medical history and implants with your provider.
Q: Can EMS replace surgery?
A: It can be an effective non-surgical option for many patients and may reduce or eliminate symptoms for some.